The following report is the most horrendous and damning VA Inspector General Report I have found.
Report No. 12-04631-313
Healthcare Inspection
Gastroenterology Consult Delays
William Jennings Bryan Dorn
VA Medical Center
Columbia, South Carolina
September 6, 2013
Executive Summary
The VA Office of Inspector General Office of Healthcare Inspections conducted a review to evaluate policies and practices related to gastroenterology (GI) consult and resource management at the William Jennings Bryan (WJB) Dorn VA Medical Center (the facility) in Columbia, SC. The purpose of the review was to determine whether deficient practices contributed to or caused delays in care, and whether facility leaders appropriately addressed clinical managers’ concerns.
We substantiated the allegations and found additional factors that contributed to the events. Veterans Integrated Service Network (VISN) and facility leaders became aware of the GI consult backlog in July 2011 involving 2,500 delayed consults, 700 of them “critical.” A funding request was made at that time and the VISN awarded the facility $1.02M for fee colonoscopies in September 2011. However, facility leaders did not assure that a structure for tracking and accountability was in place and by December, the backlog stood at 3,800 delayed GI consults. The facility developed an action plan in January 2012 but had difficulty making progress in reducing the backlog. An adverse event in May 2012 prompted facility leaders to re-evaluate the GI situation, and facility, VISN, and Veterans Health Administration leaders aggressively pursued elimination of the backlog. This was essentially accomplished by late October 2012. However, during the review “look-back” period, 280 patients were diagnosed with GI malignancies, 52 of which had been associated with a delay in diagnosis and treatment. The facility completed 19 institutional disclosures and 3 second-level reviews are still pending. As of May 2013, nine patients and/or their families had filed lawsuits.
A confluence of factors contributed to the GI delays and hampered efforts to improve the condition. Specifically, the facility’s Planning Council did not have a supportive structure; Nursing Service did not hire GI nurses timely; the availability of Fee Basis care had been reduced; low-risk patients were being referred for screening colonoscopies, thus increasing demand; staff members did not consistently and correctly use the consult management reporting and tracking systems; critical VISN and facility leadership positions were filled by a series of managers who often had collateral duties and differing priorities; and Quality Management was not included in discussions about the GI backlogs.
The GI consult backlog has been the subject of multiple reviews and recommendations, and overall, the conditions have improved and the GI backlog has resolved. However, continued vigilance is needed to ensure that the conditions do not recur. We recommended that the VISN, in accordance with the Administrative Investigative Board conclusions and recommendations, take appropriate action in relationship to facility leadership deficits contributing to the GI consult backlog.
The VISN Director concurred with our recommendation and provided an acceptable action plan. (See Appendixes A, pages 15–17 for the Director’s comments.) We will follow up on the planned actions until they are completed.
JOHN D. DAIGH, JR., M.D.
Assistant Inspector General for Healthcare Inspections
Read Entire Report Here
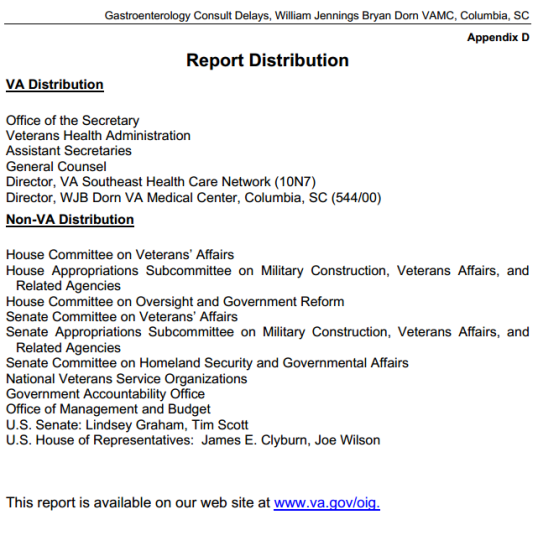
When the VA Office of the Inspector General – OIG conducts this type of Inspection, the Final Report is then distributed. At the end of the Report is the Distribution List.
This Report was Distributed to the Following:
Appendix D
Report Distribution
VA Distribution
Office of the Secretary
Veterans Health Administration
Assistant Secretaries
General Counsel
Director, VA Southeast Health Care Network (10N7)
Director, WJB Dorn VA Medical Center, Columbia, SC (544/00)
Non-VA Distribution
House Committee on Veterans’ Affairs
House Appropriations Subcommittee on Military Construction, Veterans Affairs, and
Related Agencies
House Committee on Oversight and Government Reform
Senate Committee on Veterans’ Affairs
Senate Appropriations Subcommittee on Military Construction, Veterans Affairs, and
Related Agencies
Senate Committee on Homeland Security and Governmental Affairs
National Veterans Service Organizations
Government Accountability Office
Office of Management and Budget
U.S. Senate: Lindsey Graham, Tim Scott
U.S. House of Representatives: James E. Clyburn, Joe Wilson
As you can see from the Distribution List not only was the Report sent to the OMB Office at the White House it was sent to every Congressional Committee having Jurisdiction and Oversight of the VA. If anyone on the Distribution list claims to have not known about the Situation at Dorn VA Medical Center, WHY NOT?
None of the Leadership of Dorn VAMC was disciplined appropriately. Only the Center Director and Chief of Staff were replaced, but not Terminated.
- Rebecca Wiley, Former Medical Director of Dorn VA Medical Center, has since Retired
- Barbara Temeck, M.D., Former Chief of Staff of Dorn VA Medical Center, Currently Practicing Medicine St. Louis VA Medical Center
- Ruth Mustard, RN, Current Director for Patient Care/Nursing Services of Dorn VA Medical Center,
- David L. Omura, Current Associate Director of Dorn VA Medical Center
- Jon Zivony, Current Assistant Director of Dorn VA Medical Center,
The VA suffers from systemic problems which have been identified many times over the decades. Very rarely is anyone held accountable or does anyone take responsibility as can be seen by the situation at Dorn VAMC.
VETERANS DIED.
As a 21+ year Veteran of the US Army and Army National Guard, I am just too angry to detail everything. But I will say I am tired of the “well we fixed it” attitude of the VA while no one is held accountable. The VA is NEVER “fixed”.